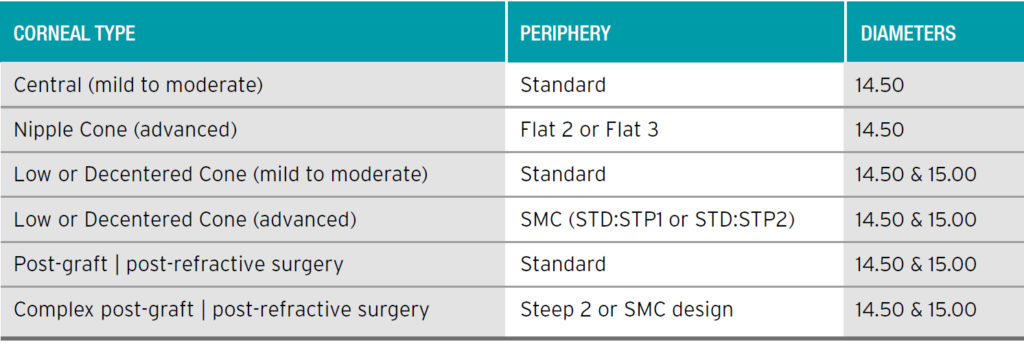
First Choice Lens – Diameter
We recommend different diameters depending on the condition. The reduced overall thickness of KeraSoft Thin improves drapage over the cornea and reduces the need for peripheral changes. More complex shapes such as post graft and low cones benefit from larger diameters.
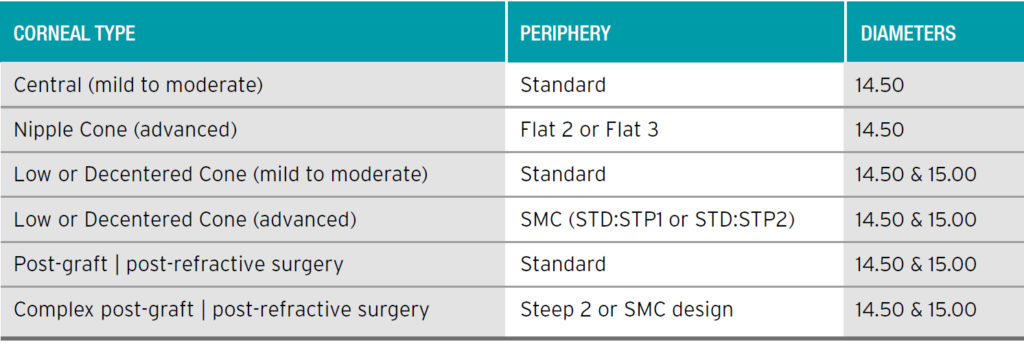
The guide below indicates where larger diameters or different peripheries are indicated.
Assessing the lens straight away
It is very important that the trial lens is observed on slit lamp immediately after insertion and the fitting assessment made within the first five minutes.
It is not recommended that the patient be sent out to let the lens settle for 15 minutes or more.
This is important for the following reasons:
- Issues such as bubbles under the lens or fluting edges can be seen immediately – these can settle and disappear after a few minutes.
- Soft lenses do not maintain their initial fitting characteristics over time. Lenses flex, stretch and settle – for example, a really flat lens can, over time, mould to the eye and bind to the surface, mimicking a tight lens.
- The fitting guidance is based on the initial assessment being within the first five minutes and thus designed to minimise chair time and improve accuracy of fitting.
MoRoCCo VA
Fit assessment is carried out by assessing Movement – Rotation – Centration – Comfort – VA
All these characteristics work together to indicate whether a fit is steep, flat or optimal.
If the fit appears Tight or Flat, remove and choose the next appropriate base curve. If fit appears Optimal, move straight to over-refraction, using the spectacle refraction as the starting point. If this is difficult to obtain, use the topography astigmatism as a starting point.
Over-refraction
Always assess the over-refraction straight away. Leaving lenses to settle for an hour or so will change fitting characteristics. Use 0.50DS steps or more when assessing sphere and cyl. It is often easier to assess the cyl before finalizing sphere correction, as large amounts of uncorrected astigmatism cause excessive ghosting.VA with a Tight lens will be better after the blink. VA with a Flat lens will be worse after the blink. VA should be atleast the same or better than spectacle refraction. If you attain a worse result, this means the fit is not optimal
MAKING PERIPHERY CHANGES
Always use STD lenses before trying a lens with a different periphery.
Each periphery change is equivalent to 0.20 change in Base Curve.
NIPPLE CONES
If the First Choice Lens Rule gives a relatively flat Base Curve (eg. 8.60) and this is acting very fl at, use that value as the peripheral fit and go down at least 2 steps for the Base Curve (ie. 8.20 FLT2).
REVERSE GEOMETRY CORNEAS
Topography does not tend to record the peripheral cornea, so the First Choice Lens Rule is likely to provide a lens that fits the central cornea but tends to flute at the edge.Keep the Base Curve as it is and tighten periphery by 1 or 2 steps or increase diameter to 15.00.
Kerasoft training overview
Download the KeraSoft Training PowerPoint presentations from our box account